Losing AHCCCS/ Medicaid health coverage in Arizona? Here’s what to do now
- March 17, 2023
- Posted by: Chad Lehrman
- Category: Arizona Health Insurance

Enrollment in AHCCCS, Arizona’s Medicaid program for low income residents, is at an all-time high of more than 2 million members. 30% of Arizona residents are now enrolled.
There are several reasons that enrollment in AHCCCS is at a record high, including COVID and loss of employment. However the biggest factor is that there is a federal Coronavirus relief law that prevents the state of Arizona from disenrolling people from the program.
Since March 2020, you cannot be taken off AHCCCS unless you die, move out of state, or ask to be disenrolled. In other words, you could be making a million dollars a year and keep getting free health coverage from AHCCCS.
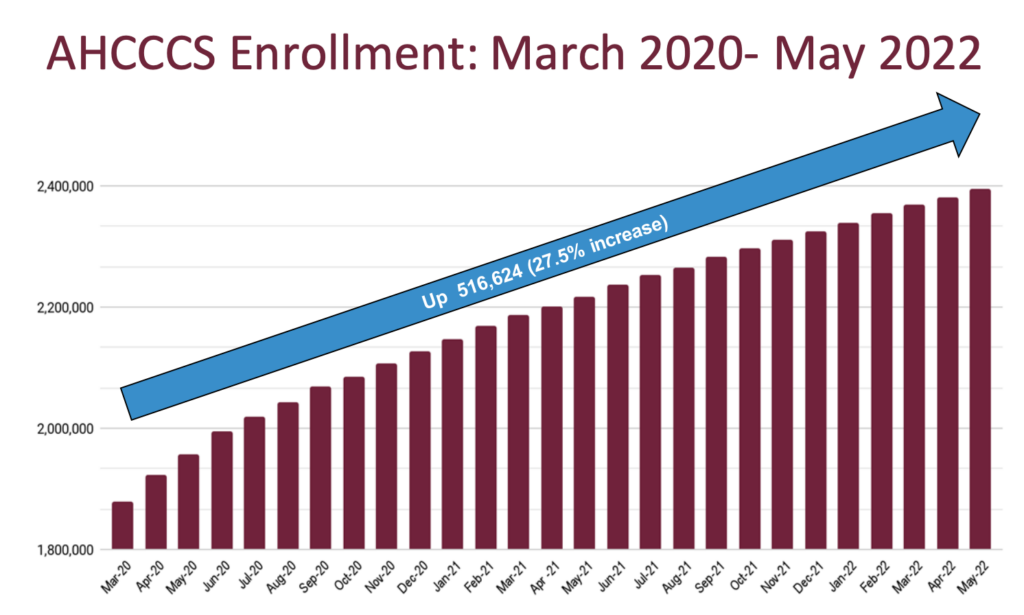
Once the COVID-19 Public Health Emergency ends, AHCCCS will begin disenrolling members who no longer qualify. They have an unwinding plan and they estimate that 600,000 members will lose coverage when the Public Health Emergency ends. AHCCCS expected the PHE to end in summer 2022, but it has been extended multiple times since then. The Biden Administration recently announced that the Public Health Emergency is finally ending.
Beginning April 1, 2023, AHCCCS will begin disenrolling members who are determined to be no longer eligible.
Getting Health Insurance in Arizona after losing AHCCCS coverage
If you are one of the estimated 600,000 people who are losing AHCCCS/ Medicaid, you have several options to find new health coverage.
1. Find individual health insurance coverage in Arizona.
Plans are available from the Health Insurance Marketplace (Obamacare/ACA plans) as well as private non-Obamacare options. Depending on your income, you may qualify for a monthly tax credit that makes the plan very inexpensive. Get free help finding a plan for you and your family by filling out our online quote request form. Or give us a call at 623-455-6997 in the Phoenix area or 520-760-0392 in the Tucson area. Open Enrollment ended January 15th, but losing AHCCCS/ Medicaid coverage is a “qualifying life event” that allows you to enroll outside of the annual Open Enrollment period.
2. Get covered under your employer’s group health insurance plan.
If your employer (or your spouse’s employer) offers health insurance, ask about joining the plan. Businesses with 50 or more full-time employees are required to offer health insurance to full-time employees. Employers are required to pay at least 50% of the monthly cost for employees, but are not required to contribute to the cost for dependents. It may be cheaper for you to decline group coverage and enroll in an individual plan.
3. Verify that you still qualify for AHCCCS.
If you still qualify for Medicaid based on their income limits and receive a notice about renewal, send them an update with your current income information.
At Lehrman Group, we have been helping Arizona individuals and families since 1988. Get in touch with us for free help finding the best plan for you and your family in Phoenix, Tucson, or anywhere in Arizona.

